Is It Possible to Get Dry Socket 5 Days After Wisdom Teeth Extraction?
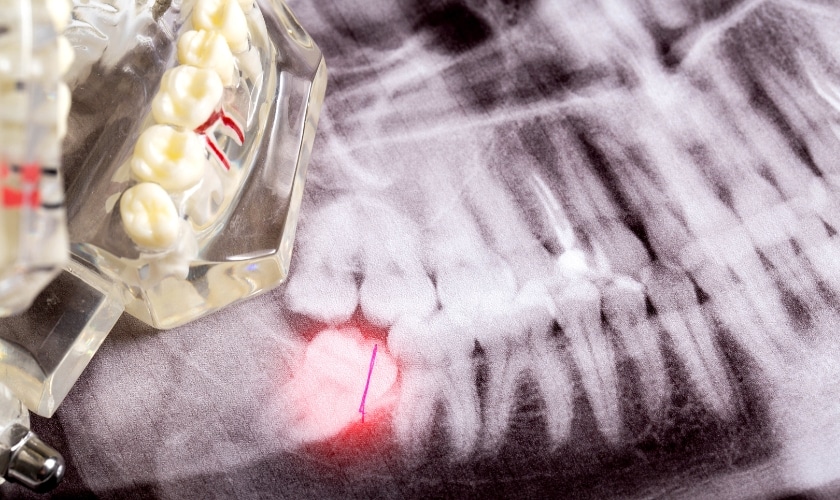
Wisdom teeth, also known as third molars, often emerge in your late teens or early twenties, sometimes causing overcrowding and impacting your other teeth. While the procedure itself is relatively straightforward, one complication that patients often worry about is dry socket, also known as alveolar osteitis. Dry socket occurs when the blood clot that forms after tooth extraction dislodges or dissolves prematurely, exposing the underlying bone and nerves to air, food particles, and bacteria. This condition can lead to intense pain and discomfort, extending the recovery period. In this beginner’s guide, we’ll delve into the possibility of developing dry socket five days after wisdom teeth extraction, its causes, symptoms, treatment, prevention, and other essential aspects often overlooked by many sources.
Introduction to Wisdom Teeth Extraction and Dry Socket
Wisdom Teeth Extraction:
Wisdom tooth extraction is a common dental procedure carried out by dentists or oral surgeons. It involves removing the wisdom teeth, usually due to:

- Impaction: when teeth are unable to fully erupt due to a lack of space, causing pain, infection, or damage to nearby teeth.
- Overcrowding: Wisdom teeth can push other teeth out of alignment, affecting your bite and aesthetics.
- Infection or damage: Wisdom teeth can be susceptible to cavities or gum disease, necessitating extraction.
Dry Socket:

Dry socket, also known as alveolar osteitis, is a painful post-extraction complication that occurs when the blood clot protecting the empty socket dislodges or fails to form. This exposes the underlying bone and nerves, leading to:
- Intense pain: Throbbing or radiating pain in the jaw, ear, or cheek.
- Bad odor: Foul-smelling breath or discharge from the socket.
- Delayed healing: Delayed wound closure and prolonged discomfort.
Causes of Dry Socket
Dry socket occurs when the blood clot at the site of the extracted tooth either fails to form correctly, becomes dislodged, or dissolves prematurely. Several factors contribute to the development of dry sockets:
- Trauma during Extraction: Excessive trauma to the extraction site during the procedure can disrupt blood clot formation.
- Poor Oral Hygiene: Inadequate oral hygiene practices post-extraction, such as smoking, vigorous rinsing, or using a straw, can dislodge the blood clot.
- Bacterial Infection: Bacterial contamination of the extraction site can lead to infection, which may interfere with proper blood clot formation.
Symptoms of Dry Socket
Identifying the symptoms of dry socket is crucial for timely intervention. While some degree of discomfort is expected after tooth extraction, the following symptoms may indicate the presence of a dry socket:
- Severe Pain: Intense and throbbing pain that radiates from the extraction site and may extend to the ear and jaw.
- Foul Odor: Unpleasant taste or odor in the mouth due to bacterial infection.
- Exposed Bone: Visible bone in the socket due to the absence of a blood clot.
- Delayed Healing: Slower than expected healing and persistent discomfort beyond the initial post-operative period.
Treatment for Dry Socket
f dry socket develops, prompt intervention is necessary to alleviate symptoms and promote healing. Treatment options for dry sockets may include:
- Irrigation: Flushing the socket with a saline solution to remove debris and bacteria.
- Medication: Pain-relieving medications or medicated dressings to alleviate discomfort and prevent infection.
- Socket Packing: Placing a medicated dressing or paste in the socket to promote healing and protect the exposed bone.
- Follow-up Care: Regular follow-up appointments with the dentist are necessary to monitor healing progress and address any concerns.
Prevention of Dry Socket
While dry sockets cannot always be entirely prevented, certain measures can minimize the risk:
- Follow Post-Extraction Instructions: Adhering to the dentist’s post-operative instructions regarding oral hygiene, diet, and activity restrictions.
- Avoid Smoking: Refraining from smoking or using tobacco products, as they can impair healing and increase the risk of dry socket.
- Gentle Oral Care: Adopting gentle oral hygiene practices, such as soft-bristled brushing and gentle rinsing with saltwater.
- Healthy Lifestyle: Maintaining a healthy diet rich in vitamins and minerals to support the healing process.
Can You Get Dry Socket 5 Days After Wisdom Teeth Extraction?
While the peak risk period for dry socket is between 3-5 days, it’s possible to develop it up to 7–10 days after extraction. The likelihood of developing dry socket decreases as the healing progresses, but certain factors may increase the risk, such as smoking, poor oral hygiene, or underlying medical conditions. Therefore, it’s essential to remain vigilant for any signs or symptoms of dry socket, even beyond the initial recovery period.
How Long Does Dry Socket Take to Heal?
With proper treatment, dry sockets typically heal within 7–10 days. The pain usually subsides within 2–3 days after treatment, and the socket gradually closes. However, complete healing and tissue regeneration can take several weeks.
Factors Affecting Healing Time:
- Severity of dry socket: More severe cases may require additional treatment and longer healing times.
- Individual healing rate: Your body’s natural healing ability plays a significant role.
- Compliance with post-operative care: Following your dentist’s instructions diligently is crucial for optimal healing.
How to Care for Your Mouth After Wisdom Teeth Extraction
- Pain management: Take prescribed pain medication as directed.
- Rest: Allow your body to rest and recover.
- Ice packs: Apply ice packs to the affected area for 15-20 minutes at a time, several times a day, to reduce swelling.
- Warm salt rinses: Gently rinse your mouth with warm salt water (1/2 teaspoon of salt in a glass of warm water) after meals and before bed to promote healing and reduce discomfort.
- Soft diet: Stick to soft, non-irritating foods during the initial healing period.
- Avoid smoking and alcohol: These substances hinder healing and increase infection risk.
- Gentle brushing and flossing: Carefully brush and floss around the extraction site, avoiding the socket itself, to maintain good oral hygiene.
- Follow-up appointments: Attend scheduled follow-up appointments with your dentist to monitor healing and address any concerns.
Conclusion:
Tooth extraction in Riverside is a common procedure, but a dry socket can be a painful complication. By understanding the causes, symptoms, and treatment options, you can be prepared and proactive. Remember, early diagnosis and prompt treatment are key to minimizing discomfort and ensuring a smooth recovery. We encourage you to discuss any concerns with your dentist in Riverside before and after your wisdom teeth extraction. We are committed to providing personalized care and ensuring your well-being throughout the process.
FAQs:
1: Can you drink through a straw after wisdom tooth extraction?
It’s best to avoid using a straw for the first few days after wisdom tooth extraction to prevent dislodging the blood clot and risking a dry socket. Stick to drinking from a cup or glass until advised otherwise by your dentist.
2: How long does it take for wisdom tooth extraction swelling to go down?
Swelling typically peaks within 48 hours post-extraction and gradually reduces over the following week. Using ice packs and following post-operative care instructions can help alleviate swelling and promote healing.
3: What foods can I eat after wisdom teeth extraction?
Stick to soft, easy-to-chew foods like mashed potatoes, yogurt, soup, scrambled eggs, smoothies, and applesauce in the days following wisdom teeth removal. Avoid hard or crunchy foods that could disrupt healing.
4: How long does it take for wisdom teeth extraction pain to go away?
Pain usually peaks within the first few days post-extraction and diminishes over the next week or two. Follow your dentist’s prescribed pain medication, use ice packs, and adhere to post-operative care guidelines for pain management.




